

First of all, it's important to understand what exactly your birth control is. Yes, it's a method of contraceptive that prevents you from getting pregnant, but how each method works, as well as the reality of the side effects, pros, and cons for each is different. So, here's the breakdown.
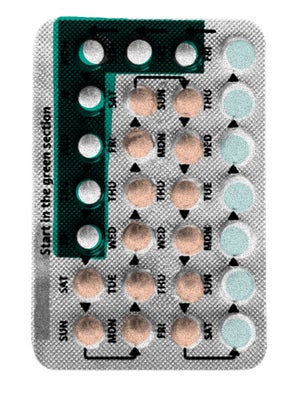
The Pill
One of the most common methods of birth control, this is a hormonal approach that uses progestin and estrogen to arrest ovulation. According to Dr. Lanskowsky, it prevents the body from ovulating by creating an environment that is similar to pregnancy. When a woman is pregnant, she doesn't ovulate, so mimicking that environment means that women on the pill cannot get pregnant. Unfortunately, that means a lot of the side effects women on the Pill experience are similar to pregnancy side effects: water retention, breast tenderness, headaches, bloating, nausea, and breakthrough bleeding. The severity of these effects depends on the dosage, the way the hormones are administered, and a woman's individual response to hormones. There are two different types of pills: Cycled pills and monophase. Cycled pills, like Ortho Tri-Cyclen, are made to mimic your cycle, so you see a fluctuation in hormone levels. Monopahse pills produce a steady rate of hormones, so the emotional ups and downs aren't quite so bad. Pros of the pill include reliable cycle control and the fact that it's a proven method that's been tried and tested. But, since the pill needs to be taken daily, even missing a single day can mean you're at risk for pregnancy. "The less often you have to do something, the better," says Dr. Lanskowsky. "The more you can remove the human error equation, the better." Which leads us to...
The Ring
Another method of hormonal B.C., this involves inserting a hormone-filled ring into your vagina, where the hormones are absorbed directly into your bloodstream. "When you take a pill, it has to be absorbed by
your intestinal tract, through the liver and into the body," says Dr. Lanskowsky. "This can cause fluctuations in hormones, which can be uncomfortable for some women and can be responsible for those aforementioned side effects. The ring functions more locally, so you have a lesser chance of suffering from these side effects." Of all the methods we discussed, Dr. Lanskowsky said that Nuvaring was the method he not only prescribed the most, but the one he saw the most patient satisfaction with. While many women are happy with this method because it cuts down on the common side effects the pill can cause, Dr. Lanskowsky does mention that many women may not be comfortable with this method since it involves insertion into the body.
The Injection
Depo-Provera, also called the birth control shot, is a longer-lasting method of birth control that also lowers the risks of side effects. The shot is estrogen-free, while most other hormonal methods of birth control contain progestin and estrogen. According to Dr. Lanskowsky, many women are sensitive to estrogen, which is the culprit behind many of the unpleasant side effects of hormonal birth control. "We add estrogen to pills because it helps stabilize the lining of the uterus, so you get less staining and breakthrough bleeding, plus it increases the effectiveness when in pill form, but you don’t need it in the injectable." The injection lasts for three months, making it a good option for people who don't want to deal with the hassle of daily or monthly birth control. Unfortunately, if your body has a bad reaction to the hormones — which can happen for some women — it's not quite so easy to get off of it. "If you have side effects with the pill, you can stop taking it. hassle-free. With the injectable, if you have side effects, you have to wait three months for it to wear off," he says.
The Implant
The next step up would be the implant, a matchstick-sized rod that is inserted under the skin of your arm. It can protect you against pregnancy for up to three years. Again, while it is reliable because you don't have to remember to take a pill every day, if you experience side effects or have issues with this method, you have to go to your doctor and have it surgically removed. There's also the risk of minimal scarring, which turns many women off of this method.
An IUD is a non-hormonal, T-shaped device that is inserted into the uterus and can prevent pregnancy for up to 12 years. There are two types of IUDs: a copper option and a progesterone option. According to Dr. Lanskowsky, IUDs have a bad rap, thanks to something from the '60s called the Dalkon Shield. "IUDs have a thin fishing line that sticks out of the cervix," he says. "The string is there so we can retrieve the IUD when it is done. The string on the Dalkon Shield had a braided string, which would create an abscess because the braids held onto bacteria. Doctors and patients both thought IUDs were terrible because they killed people, but it wasn't the IUD — it was the string." Because of this unfortunate incident, it's taken IUDs a long time to recover from the bad press and people are still hesitant to trust them, even though they are one of the most effective methods of birth control available. Again, the downside of this method is that if your body reacts negatively to the device or it migrates into your uterus, you have to have it surgically removed. Otherwise, it is easily removed by your doctor in an outpatient procedure.
The misinformation floating around about birth control is staggering — part of that can be blamed on the political investment in the issue, across the spectrum (and the opportunity for basically any talking head, regardless of qualification, to find a soapbox somewhere in the 24-hour news cycle), but part of it can also be blamed on a lack of readily available information. While we learn the basics of birth control in school, rarely do teachers go in-depth on the nitty-gritty details that would clear up a lot of general confusion. Here, we've gathered some of the most common myths we've heard, and asked both doctors just how true they really are.
Plan B is an abortion pill.
Completely false. "There are a lot of people who make that argument and are deliberately trying to confuse what is happening — they equate it with medication abortion," says Dr. Lesnewski. "Medication abortion is a pill that ends pregnancy. Emergency contraception is a pill you take after sex to lower your chances of getting pregnant — it does not terminate or hurt a pregnancy. If you were pregnant already and didn’t know it and took emergency contraception, it just wouldn’t work."
IUDs work by causing you to have a miscarriage.
Dr. Lanskowsky says this one is a big fallacy. While doctors don't all agree on exactly how the devices work, there are some theories and none of them include miscarriages. First: "Sperm have an enzyme at their head that allows them to digest the cell wall of the egg and break through to fertilize it," he says. "Copper makes that enzyme inactive, so the sperm just bounce off the cell wall and are unable to fertilize. The second theory is that it may cause a sterile inflammatory reaction, which causes the body to consume the egg as if it is a foreign body and decreases the sperm count in the uterus. And the final theory is that because the IUD is shaped like a T, at the little spot where the IUD is in contact with the uterine wall, if the pregnancy occurs, it may prevent the fertilized egg from implanting (because there is foreign body there)."
The pill will make you gain weight.
Sadly, this one is partially true. Says Dr. Lesnewski, "The only kind of birth control that we know for sure can cause women to gain weight is the injection, because it increases your appetite, causing you to eat more." Adds Dr. Lanskowsky, "Many pills can cause a 3-5 pound weight gain — usually within the the first three months of starting the pill. This water weight will usually go away after one to three months. Yasmin, a relatively newer oral contraceptive, has an ingredient that functions like a diuretic (so it purportedly will not cause this weight gain), but it requires a little more surveillance by a doctor. The real untold story behind weight gain and the pill is that progestins are an appetite stimulant — so if diet and exercise remain the same a woman should not see a huge amount of weight gain."
Going off of birth control will cause all sorts of horrible side effects, like breakouts, heavier periods, and weight gain.
While you may experience these symptoms, Dr. Lanskowsky says they aren't caused by the pill. "Women who are on birth control for a long period of time, many of them have been started on it for a reason, specifically if you were started in your early teens. You may have suffered from heavy periods, or really bad PMS. The pill will make those unpleasant symptoms stop for as long as you are on it, but it will not cure you of those problems. When you stop the pill, it is out of your system in about 24 hours, so I would think a lot of those rebound effects you hear about are symptoms that the woman had before she went on the pill. The woman would have been accustomed to living without those issues, so they may feel more severe because she's been off them for so long. It's easy to forget things that are painful. You started the pill to minimize these problems, but it's not going to fix them — it will mask them, but they are not going to improve." Bummer.
Birth control can cause cancer.
On the contrary, it can actually help prevent some forms of cancer. While breast cancer can be stimulated by hormones, those same hormones help protect women who are prone to uterine and ovarian cancer. "When a woman gets an overgrowth in the lining of her uterus, that can develop into uterine cancer," says Dr. Lanskowsky. "The combination of estrogen and progestin actually protects the lining of the uterus."
It's dangerous to be on continuous birth control for a long period of time.
According to Dr. Lanskowsky, there's no conclusive evidence that being on continuous birth control (i.e skipping our monthly periods by taking back-to-back does of hormones with no breaks in between) is harmful to your health. "There really doesn’t seem to be a downside to missing a period for months and months. We usually have a woman get a period a few times a year when they are on those regimens, but there's no medical need for it. We do that just to make sure it's still working."
Once you go on the pill, it will be harder for you to get pregnant when you go off of it.
It's probably not the pill that's causing you to have difficulty conceiving, says Dr. Lanskowsky. Many women start birth control at a very young age, then go off it later in life. "You started when you were 15 and now you are 35 and that changes things," he says. "Things haven’t stayed the same for that person over the 20 years they've been on birth control, so their weight and stress are not the same. If you can’t get pregnant, it’s not the pill." Basically, it's your age that is causing the difficulties. His advice? Once off the pill, you have to re-learn your cycle lengths in order to best gauge fertility and when your body is the most receptive to fertilization. It may take your body a bit of time to get back into a rhythm after being aided by hormones for so long, but it will get there — just be patient.
Going on and off birth control is dangerous.
According to Dr. Lesnewski, the only danger of going on and off birth control is the risk of unintended pregnancy. "A lot of times when women go off the pill, they don't go on another method of contraception and then they get pregnant."
If you go on birth control, you are at serious risk of getting life-threatening blood clots.
While rare, blood clots are definitely a risk associated with taking birth control, especially if you are a smoker. "Any kind of birth control that contains estrogen can cause blood clots. Bottom line is that blood clots can happen, but they are very rare. They go from being super, super rare to a little less rare for women who are taking hormones," says Dr. Lesnewski.
People with migraines should not use birth control.
Once again, this one has some truth to it. "Women with migraines, especially with aura, are not supposed to take any birth control that contains estrogen," says Dr. Lesnewski. "Women who have just plain old migraines can use estrogen. Because those who suffer from auras are at a higher risk for stroke, the World Health Organization has concluded that the extra risk is not worth it — there are so many other methods they can use."
There's a big difference between all the different brands of pills.
Not to be cynical, but Dr. Lanskowsky says this is all a ruse perpetuated by the drug companies. "There's no reason to have 100 brands of birth control. All these little subtle differences between pills, that really has to do with their loss of brand status. Now that pills have become generic, the FDA allows for minimal changes to rebrand a pill so it's no longer generic because it’s a brand name. Generally, when you are taking about mono-phasing pills or tri-cycle pills, the core ingredients aren’t very different. You are rarely going to see huge benefits [from switching]. A lot of this is just advertising. 'The only pill approved for acne prevention?' That has nothing to do with that pill — it's just that they are the only ones that sought FDA approval to market their B.C. as an acne pill."

And that brings us to the current heated debate over birth control. After Obama's PPACA passed, one of the main pieces that was being hotly contested was the part that required insurance companies to cover contraceptives at no cost to consumers. While we think a little bit of research and reading makes it pretty clear that insurance companies, in the long-term, aren't losing money on this initial spend, we have seen a lot of protest coming from the conservative end of the spectrum about both the financial burden on insurance companies and on the government, as well as concerns about the morality of contraception.






